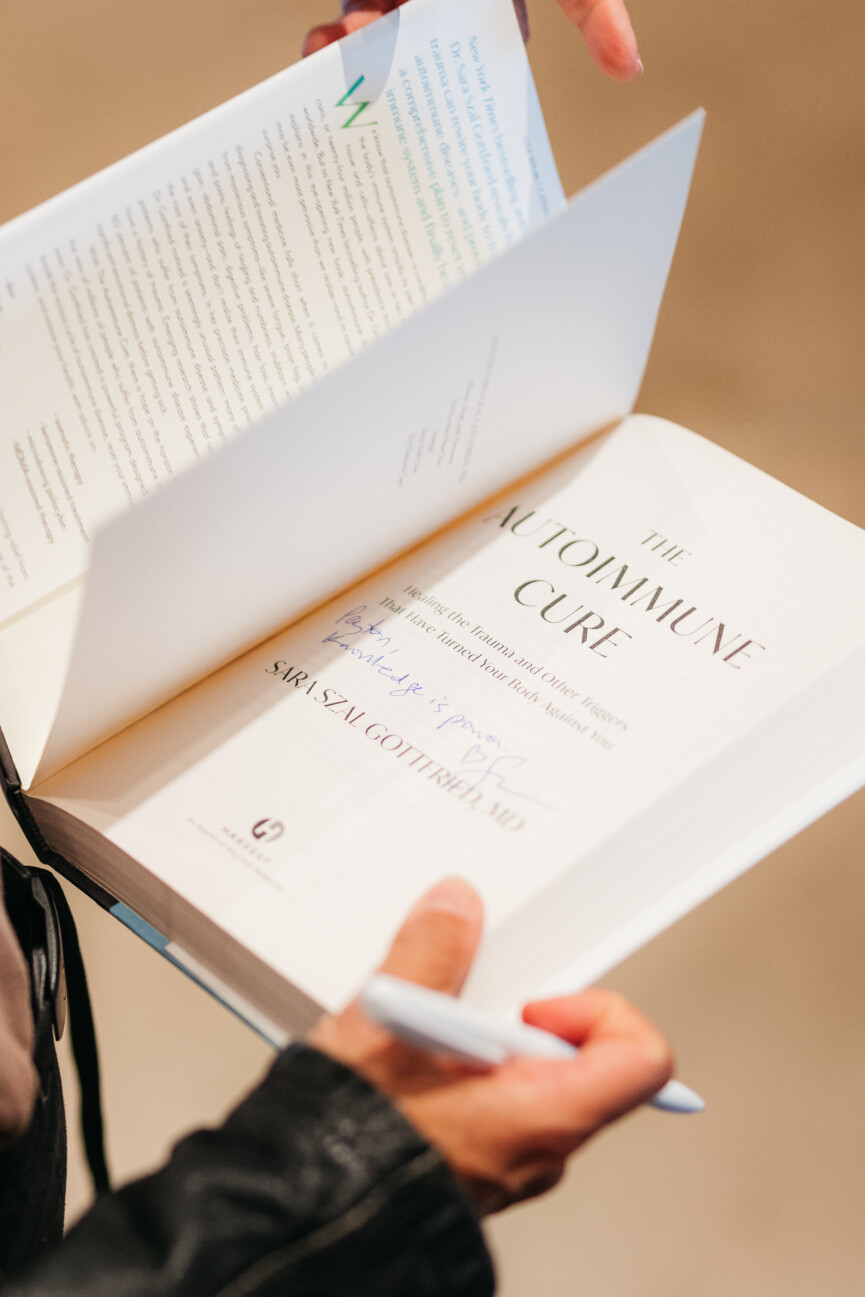
There were about 15 of us bobbing about the freshwater pool at WorldSprings, a mineral hot springs spa in Dallas, Texas. We were there, ostensibly, for a floating sound bath, but our eyes continued to gravitate toward Dr. Sarah Gottfried throughout the meditative experience. Even dressed down in a bathing suit and sunglasses, you could sense the gravitas of a four-time New York Times bestselling author. The board-certified physician, who graduated from Harvard and MIT, was visiting the Dallas destination (where she serves as WorldSprings’ Wellness Advisor) to partake in the sound bath, guide us through an anti-inflammatory circuit of saunas, cold plunges, and mineral baths, and sign her latest book, “The Autoimmune Disease Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against You.” Most of us were there for her.
Featured image by Riley Blanks Reed.


Autoimmune Disease and Trauma: A Conversation on This Surprising Connection
Fangirling began as soon as the sound bath ended. “Your work changed my life” was the resounding sentiment. Dr. Gottfried’s books have addressed everything from hormonal detoxification to slowing the aging process, with a throughline of taking control of your health—particularly as a woman. “Don’t give your power away to your doctor or nurse practitioner,” Dr. Gottfried shares with me. “No one will know your body like you do.”
“Don’t give your power away to your doctor or nurse practitioner. No one will know your body like you do.” – Dr. Sara Gottfried
Dr. Gottfried’s latest book focused the researcher’s attention on autoimmune diseases, which have dramatically increased in recent years, particularly among women. She suggests a surprising cause.
“I found a massive rise in autoimmunity in my practice during the pandemic, and it seemed that the rise of trauma was at the root of it,” Dr. Gottfried shares. “I listen to what my patients tell me, and this was the narrative in my practice from hundreds of patients: more trauma and more autoimmunity.”
After a circuit of saunas, cold plunges, and globally-inspired soaks, I spoke with Dr. Gottfried to dig a little deeper into her latest work. The noted doctor shares her thoughts on adverse childhood experiences (ACEs), phsychadelic therapy, and the supplement most women probably need to be taking.

Dr. Sara Gottfried is a four-time, New York Times bestselling author on innovative integrative health topics. She is a Harvard- and MIT-educated physician, speaker, yoga teacher, and author. She is a Clinical Assistant Professor in the Department of Integrative Medicine and Nutritional Sciences at Thomas Jefferson University, where she is Director of Precision Medicine at the Marcus Institute of Integrative Medicine.

What first pointed you to investigating trauma as a trigger for autoimmune disease?
The three requirements for developing autoimmune disease are genetic predisposition, leaky gut, and a trigger. The trigger can be sweeping hormonal change such as postpartum or perimenopause or menopause. It can also be infection, like Covid, or a traumatic experience. It can be loneliness or isolation. I found a massive rise in autoimmunity in my practice during the pandemic, and it seemed that the rise of trauma was at the root of it.
Is there a particular kind of trauma that tends to trigger autoimmune disease?
The type of trauma that has been investigated the most is adverse childhood experiences (ACEs), or experiences of abuse, neglect, or other difficulty in childhood. You can learn your ACE score here.
Autoimmune disease disproportionately affects women. Why do you think that is?
Women experience approximately 10% more trauma than men according to the ACE studies. We also have more significant hormonal changes in pregnancy, postpartum, and in perimenopause and menopause. Hormones modulate the immune system. Those are sex differences. There are also gender differences that are socially constructed that can rob women of health and increase their risk of autoimmunity, such as having more caregiver demands and getting paid less for equal work. All of these factors can contribute to women’s greater risk of autoimmune disease, such that four out of five people with autoimmune disease are women.
I loved your discussion with Dr. Mark Hyman about different types of psychedelic therapies. How do you feel they differ from traditional talk therapy when it comes to treating trauma?
Psychedelic-assisted therapy is different from traditional talk therapy in that it seems more effective at resolving post traumatic stress disorder. Talk therapy has an effectiveness of about 30% at resolving PTSD. One form of psychedelic therapy, MDMA-assisted therapy, has an efficacy of 67% to 71%, so it is more than twice as effective. Psychedelic-assisted therapy has been shown to be helpful in preliminary studies for multiple conditions, including treatment-resistant depression, end-of-life care, and disordered eating.
What would you tell someone who has never tried psychedelic therapies? How did they benefit your own healing journey?
We are still in the early stages of understanding the benefits of psychedelic therapies, even though many of the traditional psychedelics have been used for thousands of years. In terms of whether to consider having psychedelic treatment, it’s important to know that despite the “just say no” anti-drug campaign, psychedelics are safer than alcohol. There are other ways to achieve healing states of consciousness, such as with holotropic breathwork, as I describe in “The Autoimmune Cure.”
In my experience, psychedelic-assisted treatment is an accelerator in the process of healing from trauma.
Can you explain the Pine System and trauma’s correlation to it?
Trauma can get lodged in the body, specifically, the psycho-immune-neuro-endocrine—or PINE—system. The PINE system describes the way you respond to your environment. This concept is sometimes described as psycho-neuro-endocrine-immunology. I prefer PINE because it’s easier to remember. PINE is a scientific area of study that investigates the bidirectional communication between the mind and its functions, the immune system, the nervous system, the endocrine system, and how they all connect to physical, mental, and spiritual health. You can consider the PINE to be your stress response system. Some of us have a very sensitive PINE system; others, less so.
What are some of your favorite wearables to track things like heart rate variability?
The wearables that I’ve found most helpful for HRV are the Oura Ring and Eight sleep, which is a system that fits over your mattress, tracks and optimizes sleep, and has helped me increase HRV more than any other.
Is there a supplement you would recommend for all women?
I don’t recommend a supplement across the board for everyone, but the one that women most commonly need is magnesium, especially if you have chronic tension. About 75% to 80% of us have an insufficiency. I usually recommend starting with 150 to 300 mg at night.
Your new book is empowering for those who want to take control of their health. What messages or advice do you hope people take away from your book?
Don’t give your power away to your doctor or nurse practitioner. No one will know your body like you do, so empowerment includes testing yourself for autoimmunity to see if you’re one of the 30% of Americans who have it.