There’s way more to wellness than just eating clean, so we’re taking a holistic approach to restoring our spaces, minds, bodies, and hearts in small but powerful ways. Introducing The RE:SET Challenge—a 21-day plan to a healthier and happier you. Click here for the full list. Next up, what is inflammation and how you can optimize your health to prevent disease with Dr. Will Cole.
A few years ago, my husband experienced brain fog. He had it for months before we eventually addressed it via an elimination diet. Turns out he had a gluten intolerance but back then, the term was very new and buzzy which meant a lot of chatter online (and a lot of misinformation) about what it is, and what causes it. Now, this underlying condition causing fuzzy thinking and an inability to concentrate is getting the medical attention it deserves.
One of the top experts in identifying and treating brain fog (among many other health concerns) is Dr. Will Cole, leading functional medicine practitioner, IFMCP, DNM, DC, and author of Ketotarian, The Inflammation Spectrum, and the upcoming book, Intuitive Fasting. He tells me one of the biggest components to “brain fog” (that many of us experience) is how healthy our gut is functioning. The gut-brain connection is well known now along with terms like “leaky gut” and “leaky brain”—yikes! In Dr. Cole’s clinic, it’s not uncommon for him to have a patient come in looking for help with depression or brain fog, and have further diagnostic testing reveal that they also have leaky-gut syndrome.
And this is where inflammation comes in. Yet another term in the wellness industry that has sparked a lot of questions. On average, there are 10k-100k Google searches for “what is inflammation” each month. What a lot of people don’t know about inflammation is how necessary it is for a healthy body to fight off infections or when you get a cut. In fact, Dr. Cole says “we would die without healthy levels of inflammation.” So, why does inflammation get such a bad rap?
Well, it’s when inflammation becomes chronic inflammation that it starts to wreak havoc on your health.
As Dr. Cole explains: “Inflammation is an important bodily process that, when triggered by factors like an unhealthy lifestyle, stress, and toxic exposures, can spin out of control. When inflammation is allowed to run wild, it can damage the body by creating too many pro-inflammatory cells and molecules, such as tumor necrosis factor (TNF), interleukins (ILs), nuclear factor-kappa B (NF-kB), prostaglandins, and free radicals. Having too many of these pesky pro-inflammatory substances being produced can cause damage to the body, leading to inflammation-related health issues and conditions, such as autoimmune disease.”
Unfortunately, a lot of people don’t even know they have inflammation until it’s too late. It’s been estimated that only 5% of people with celiac are ever diagnosed (that’s about 3 million Americans with celiac disease who have no idea that they have it) and at least 6% have gluten sensitivity or FODMAP intolerance because of chronic gut problems like small intestinal bacterial overgrowth (SIBO). So, how do we know we have issues with inflammation? And what are the main signs we should watch out for?
Of course, the answer to that isn’t simple.
“Since everyone is unique, inflammation can manifest in a variety of different ways,” Dr. Cole adds. “However, the most common symptoms I see are fatigue, brain fog, moodiness, weight loss resistance, and joint and muscle pain.”
The only way to know for sure if inflammation is an issue for you and to what extent is through lab work. Ultimately, to keep your inflammation levels low, Dr. Cole says we should avoid triggers including stress, toxin exposure, and poor dietary habits. Although, I can see how that seems like an impossible task in the world we currently live in. But, we have to try, right?
Read on to learn more from Dr. Cole about what is inflammation, ways to treat it, and how you can optimize your health to prevent disease. Oh, and be sure to scroll to the end for an exclusive anti-inflammatory recipe to try!

This seems to be the age of autoimmune, but as you said, “just because something is ubiquitous doesn’t make it normal—or mean that we can’t do something about it.” So, what can we do about it? Is it reversible? Can we heal and how?
Once you are diagnosed with an autoimmune condition, you will never fully get rid of your autoimmune condition. But you can put your symptoms into remission. By running labs and looking at the root cause of your symptoms, functional medicine aims to alleviate symptoms through dietary and lifestyle changes specific to your health case and unique biochemistry.
So, what is the auto-immune inflammation spectrum?
To be diagnosed with most autoimmune diseases, the immune system has to destroy a significant amount of tissue to be officially diagnosed. For example, there has to be 90% destruction of the adrenal glands to be diagnosed with Addison’s disease.
But let’s think about this for a minute—these diseases do not happen overnight! The truth is that diagnosis happens at the end stage of these conditions. This is why I look at autoimmunity as a spectrum. You can be on the low end, with some reactivity, or in the middle, with significant symptoms but are still not conventionally diagnosable, or you can be at the end stage, when a doctor finally says, “Yep, you have (insert disease here.)”
What are the three main stages of the auto-immune inflammation spectrum?
The three main stages of the autoimmune-inflammation spectrum including silent autoimmunity, autoimmune reactivity, and autoimmune disease. Silent autoimmunity is when there are positive antibody labs but no noticeable symptoms, autoimmune reactivity where there are positive antibody labs and symptoms, but still not enough to warrant a formal diagnosis, and finally, an autoimmune disease where there is enough body destruction to be diagnosed.
Among my patients, I find that quite a few of them are at Stage 2, about halfway along the autoimmune spectrum. They aren’t sick enough to be labeled with an autoimmune disease, but their health and bodies are, in my opinion, significantly damaged by the effects of autoimmune reactivity.

What are some of the most common early symptoms of inflammation?
Again, symptoms are going to vary between individuals however, most commonly I see fatigue, brain fog, and weight loss resistance as early signs.
How does your work in functional medicine help to discover these problems when other specialists can’t?
Functional medicine aims to uncover the root cause of why someone is feeling the way that they do. Then, we can come up with a plan to address these causes that is specific to their case. This is so important since not every person is going to respond the same way to the same treatment even if their diagnosis is identical. Functional medicine takes into account bio-individuality, unlike conventional medicine which typically just matches symptoms to a corresponding drug. However, we do see the necessity of medication for certain individuals and work in tandem to optimize a person’s health enough to eventually not need the medication or need a lower dose.
What are the main tests to consider if you have autoimmune or inflammation?
One lab I typically run on patients is what’s referred to as predictive autoimmunity. This lab allows us to see whether there is any abnormal immune response against many parts of the body. There are also a few labs that I run that look at inflammation levels:
- CRP: C-Reactive Protein is an inflammatory protein and the test measures it along with IL-6, another pro-inflammatory protein. They are both linked to chronic inflammatory health problems. Optimal Range: < 0.5 mg/L
- Homocysteine: This inflammatory amino acid is linked to heart disease, destruction of the blood-brain barrier, and dementia. This is also commonly elevated in people with autoimmune problems. Optimal Range: < 7 Umol/L
- Ferritin: Normally used to check for stored iron levels in cases of suspected anemia, it is also considered to be an acute phase reactant, and when high, it’s a sign of inflammation. Optimal Range: Men: 33-236 ng/mL; Premenopausal women: 10-122 ng/mL; Postmenopausal women: 10-263 ng/mL

A whopping 75% of people with autoimmune diseases are estimated to be women. Why are women more prone than men?
Since autoimmunity tends to present itself after stress (through increased inflammation) women tend to be more prone to men since they can undergo more stressful life events that affect the body including pregnancy. Also, women go through more hormonal changes than men that can also play a role.
What can we do today to optimize our health and prevent disease?
Since there are no “one-size-fits-all” approaches to your health, it’s important to listen to your body as much as possible. Find out what works for you. Start with an elimination diet like the one in my book The Inflammation Spectrum to discover what foods are optimal for you and learn to listen to your body through intuitive eating and fasting like in my book Intuitive Fasting.

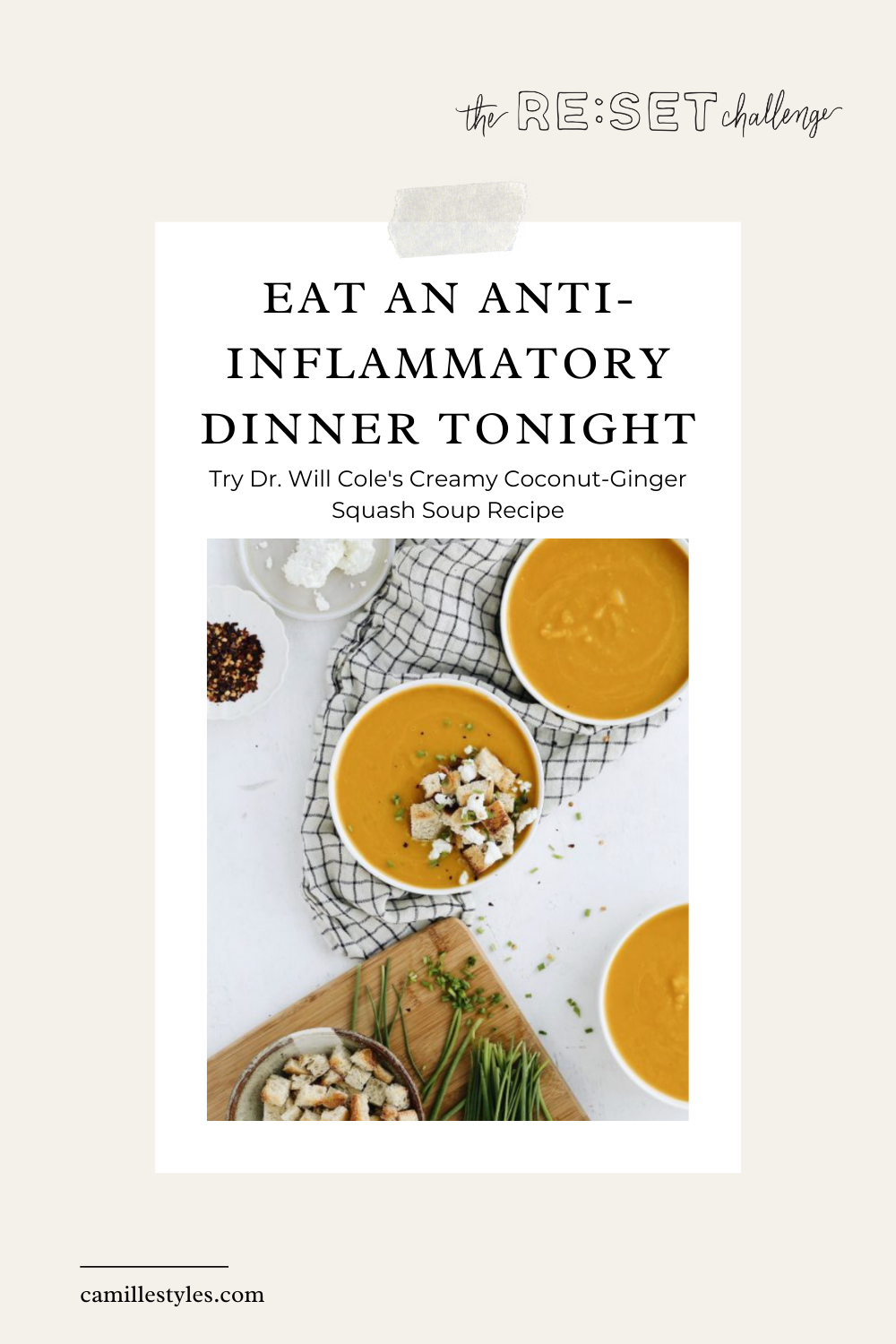
Dr. Cole’s Anti-Inflammatory Creamy Coconut-Ginger Squash Soup Recipe
Ingredients
- 2 tablespoons ghee
- 1 cup coarsely chopped yellow onion
- 1 ripe pear, peeled, halved, cored, and coarsely chopped
- 2 16oz. bags frozen butternut squash (4 cups)
- 1 tablespoon grated fresh ginger
- 1 teaspoon ground turmeric
- 1/8 teaspoon ground cloves
- 1 teaspoon sea salt
- 1/4 teaspoon black pepper
- 1 can unsweetened coconut milk
- 2 cups chicken bone broth
- Crumbled cooked bacon or Prosciutto chips
Directions
- In a Dutch oven, melt the ghee over medium heat. Add the onion and cook, stirring occasionally, for 8 to 10 minutes or until tender and caramelized. Add the pear and squash; cook until the squash is lightly browned and the pear is tender. Stir in the ginger, turmeric, cloves, salt, pepper, coconut milk, and broth. Cook, stirring frequently until heated through.
- Using an immersion blender, carefully blend the soup until completely smooth. (Or let the soup cool slightly, then carefully transfer it in batches to a food processor or blender; process or until completely smooth.) If the soup is too thick, add water, 2 tablespoons at a time, until desired consistency is reached.
- Top each serving with crumbled bacon or Prosciutto chips if desired.